AI billing for telehealth practices
End-to-end AI powered RCM for telehealth practices. Everything from VOB and prior auth to claim management
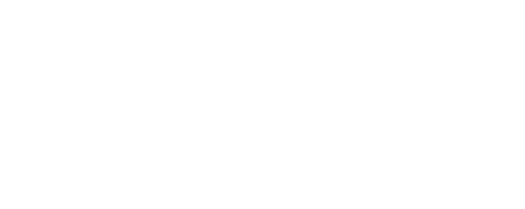
Automated VOB and Billing across 700+ payer plans






End to end touchless RCM
Immediate VOB
goodBilling uses coverage information across hundreds of fully funded and self funded plans and returns patient responsibility in seconds
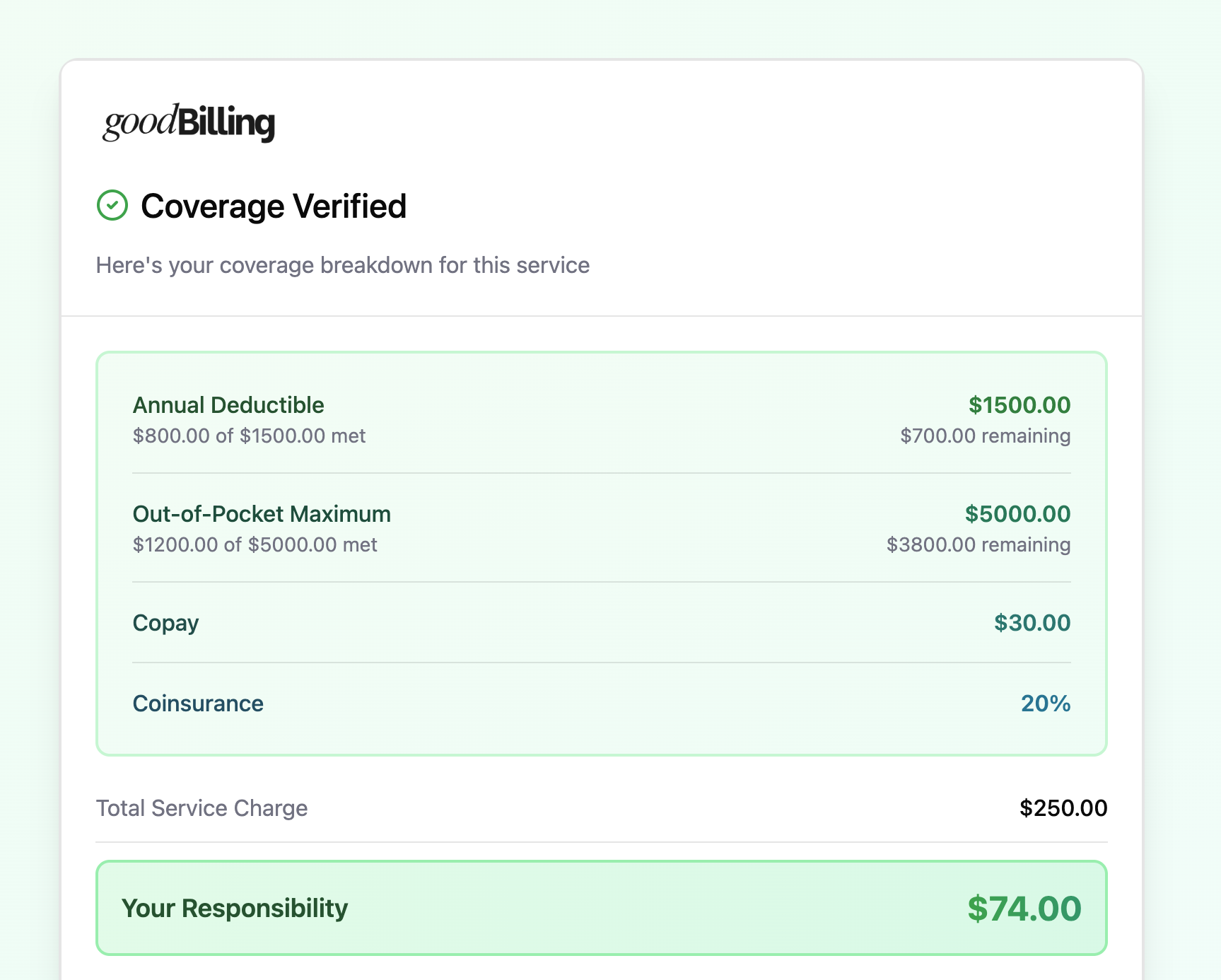
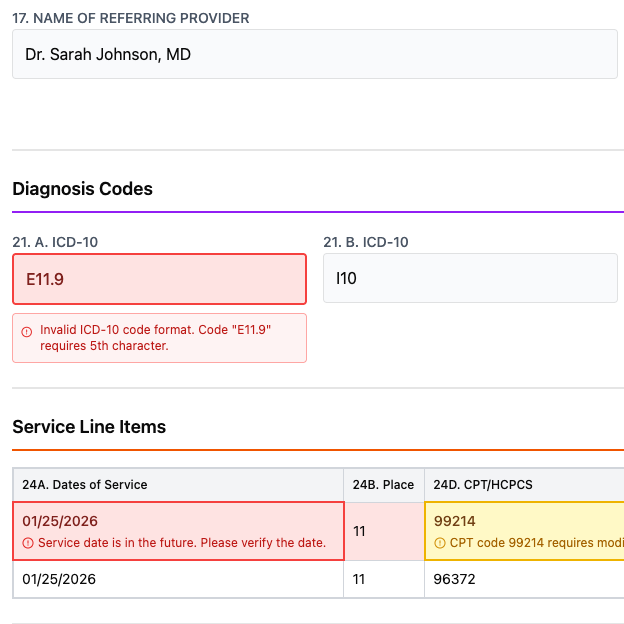
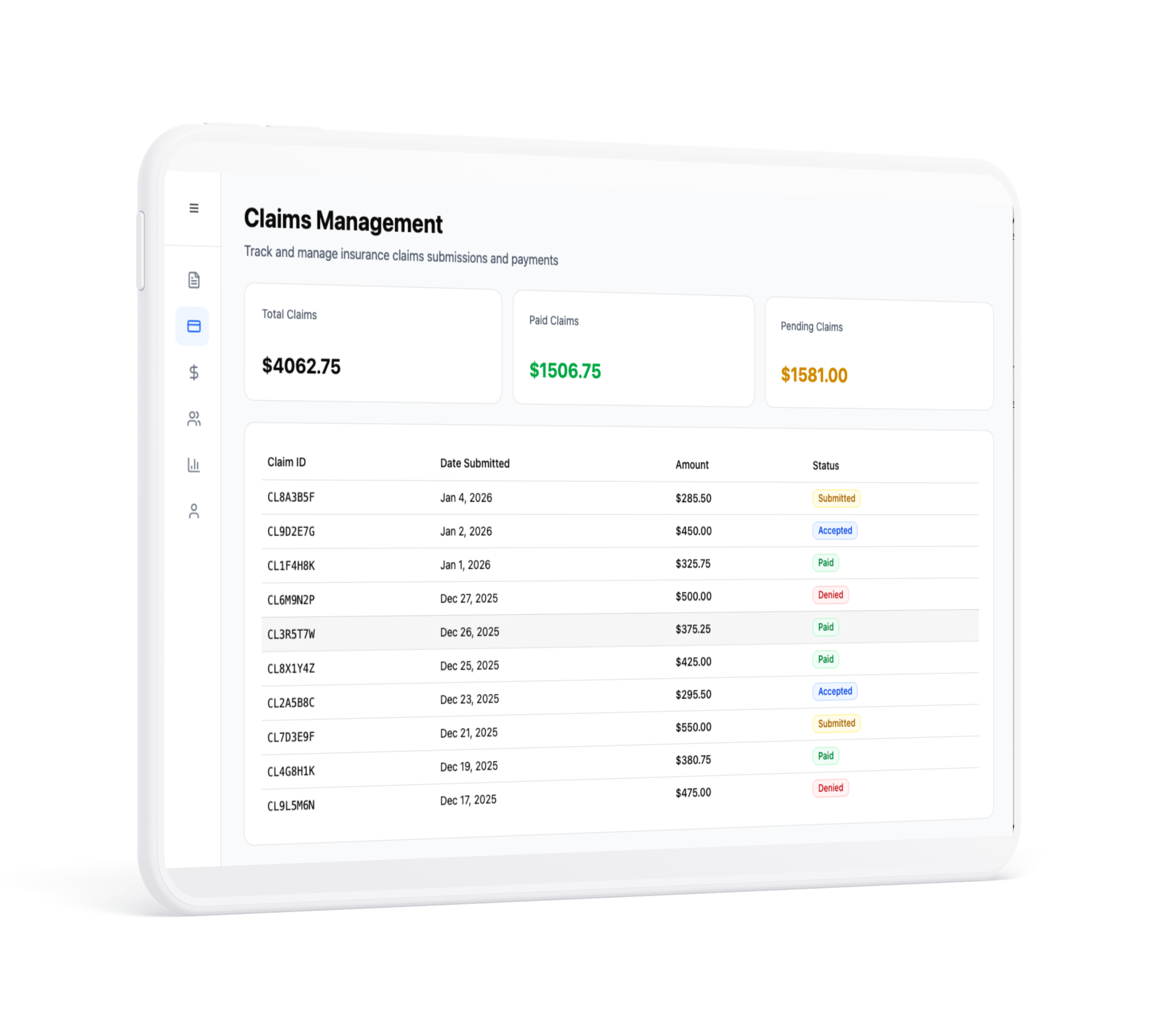
Automated claims
Claims are created, scrubbed and submitted automatically using AI analysis of clinical notes
Denial management
Denials happen. goodBilling will automatically analyze denial reasons and submit an appeal. Our goal is 0% denial rate.
Billing bliss
Regular security audits are conducted to ensure the platform adheres to the highest security standards.

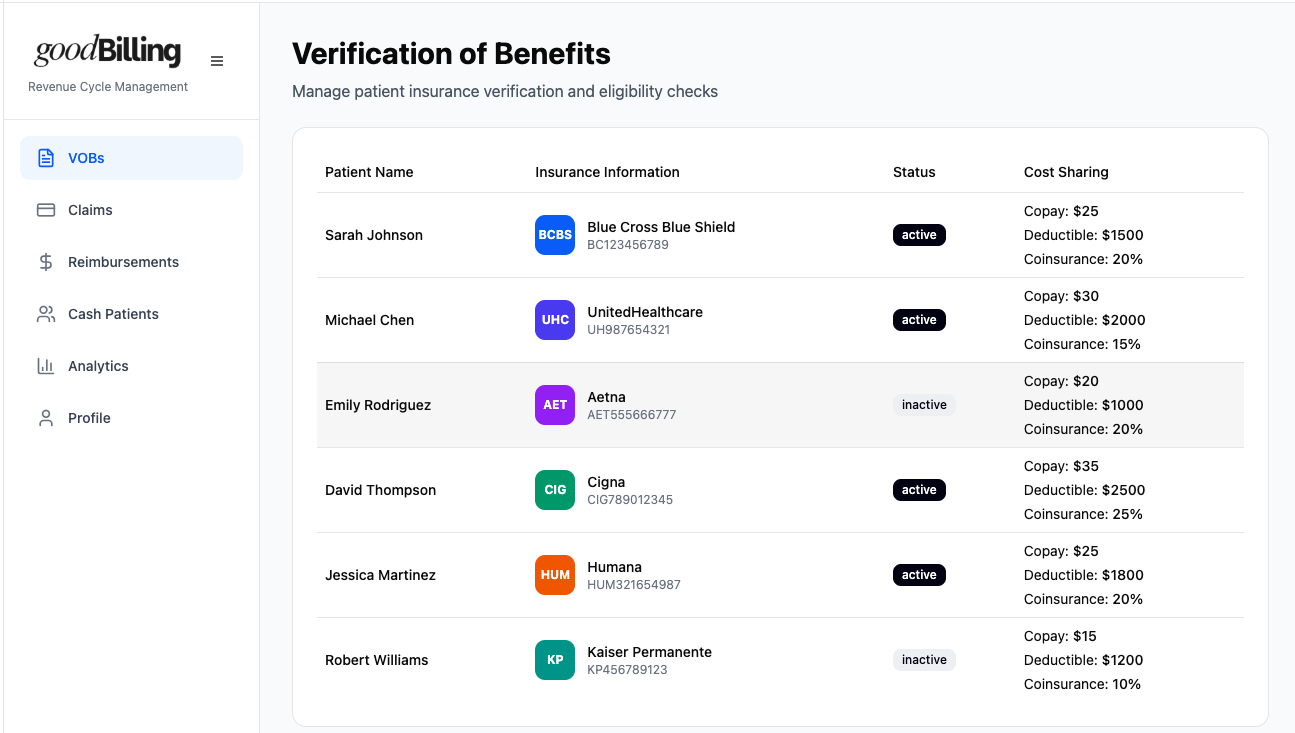
Peace of mind for your client
Clients want to know if they're covered and what their out-of-bucket responsibility is. With good billing, you can provide those answers instantly.

EMR integrations
goodBilling integrates with top EMR systems. Data exchange happens automatically and securely
Reliable revenue streams
By running a legibility check before the appointment and scrubbing the claims, we prevent denials before they even happen.

Integrated payment processing
goodBilling can handle charging and invoicing for patient responsibility automatically. No more chasing patients for outstanding bills.

AI first RCM
Agentic payer portal communcation
Our agents can automatically communicate with the payer agents and get the required coverage information, including data you cannot get from standard clearing house requests.
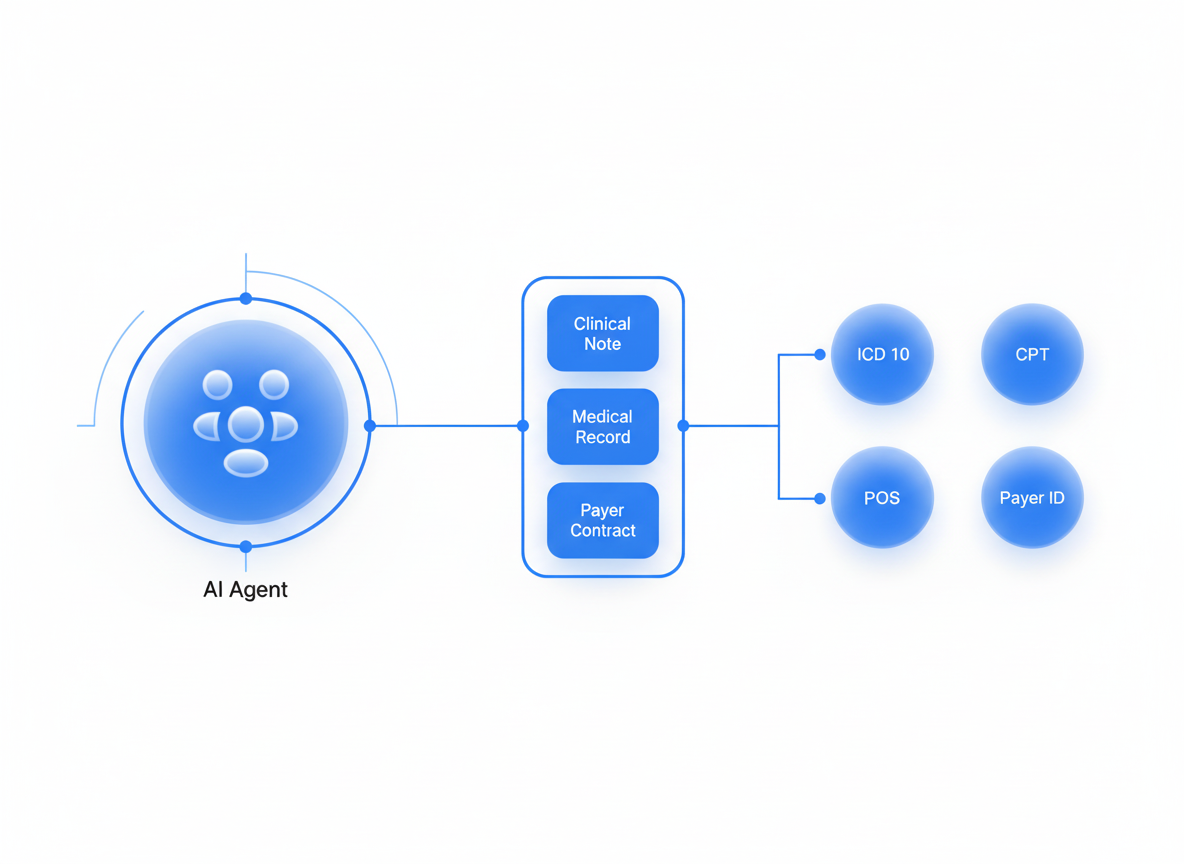
Claims on autopilot
We use AI to process medical records and payer contracts to identify the right procedural and diagnosis codes to use on the claim.
It's intuitive, efficient, and has saved us countless hours. Our team can focus on what really matters.
Since we started using goodBilling, we stopped thinking about billing and insurance companies altogether. We just focus on care.
We cut RCM costs dramatically—far below 10% fees or hiring a biller—while getting faster reimbursements.
Eligibility checks went from hours to seconds; patients get instant benefit details before we even start.
This is quite amazing! Claims submit automatically right after note signing, and denials are flagged immediately—no more weekly claim babysitting.
Trusted by hundreds of practices in the US

68K
Claims created each month

$1M+
In RCM savings delivered each month

300
Clinics onboarded
Experience the future of RCM
Talk to us today and see how goodBilling can help your practice.
.png)
.svg)